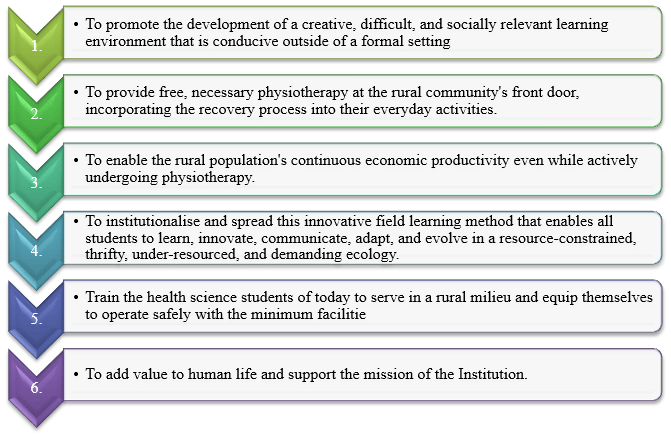
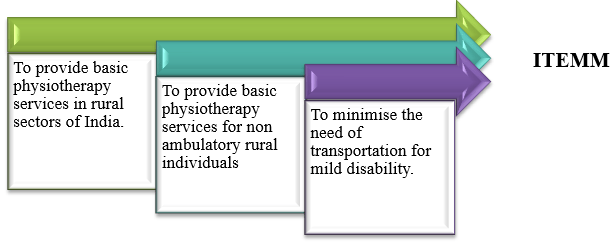
The ITEMM scheme is a pioneering journey of MAHER into unchartered territory. The data presented shows an exponential increase in the number of camps organized annually with a corresponding increase in the student participation. The number of students undergoing this hands-on experience went up from 80 to 200 annually over a period of 5 years. Feedback obtained from the students and the faculty denote that ITEMM improved their communication skills, enhanced their cooperation and team spirit, augmented their lateral thinking and reinforced their clinical skills to offer effective medical help in resource poor settings.
ITEMM is a domiciliary rehabilitation scheme and a MAHER benchmark initiative to equip the physiotherapy students with an indispensable practical tool that is socially relevant to a rural community.
Goals of the Practice
Preparatory Training: The final year students of the BPT course participated in a one-day training session, organized to sensitize and equip them for the successful implementation of the program.
Logistics Management– MAHER provided unflinching support for logistic management ensuring provision of manpower, equipment and transportation. A fully equipped mobile physiotherapy van was procured for the purpose at the cost of 30,00,000/- (Thirty Lacs) along with the equipment cost.
Community participation– The outreach team of MAHER ensured the cooperation of the leaders from the pre identified rural communities thereby empowering them towards better health and well-being.
Plan implementation– The Physiotherapy students of MAHER set up the base camp in the central village under the supervision of the faculty. The lodging arrangements were provided by the villagers while the transportation and food were sponsored by MAHER. The students fanned out to the surrounding villages in batches of ten, where all needy patients were offered physiotherapy at their doorstep. The teams visited the villages continuously for seven days ensuring absolute patient compliance.
Self-Help Stations (SHS)– the establishment of Self-Help Stations in 15 villages was done in a period of 5 years costing approximately 3,00,000 (three Lacs). The SHS were set up in a well-ventilated room of the local school and equipped with basic instruments required for rehabilitation. Patients requiring chronic rehabilitation continued their physiotherapy at the SHS. A science teacher of the school was provided with basic knowledge and training to assist the patients in obtaining physiotherapy.
Tele-support– The SHS stations were supported through tele medicine provided by the faculty of physiotherapy of MAHER for as long as was necessary.
- The number of villages covered grew from 30 in 2017-18 to 55 in the year 2021-22 and the number of patient beneficiaries grew from 1013 in 2017-18 to 2507 in 2021-22. This indicated an increasing demand for the services provided by the ITEMM scheme and an expression of confidence from the rural communities.
- This best practice fulfilled the Institutional Social Responsibility, boosted the educational atmosphere and generated social soft power for the growth of MAHER. It also reflected the credibility of MAHER and served as an important agent of positive change for the Institution and the rural society that it served.
- ITEMM thus facilitated excellent patient compliance, early recovery and return to work with minimum loss of working man days and wages.
India’s healthcare system is overburdened, underfunded, understaffed and unevenly distributed. While many diseases and conditions are well known and attract adequate medical, social, administrative and government attention, a few diseases that primarily affect the poor are largely overseen. Diseases like cleft lip and palate anomaly are predominately prevalent in rural areas where there is an acute lack of awareness and resources for multidisciplinary approach necessary for successful treatment. Many patients receive limited or suboptimal care. The existing public healthcare system is overburdened and prioritized to tackle important communicable and lifestyle diseases such as tuberculosis, AIDS, malnutrition based diseases, Malaria, Dengue, Diabetes, Hypertension, etc. The defect adversely affects not only speech and normal development of facial and oral functions, but due to disfigurement, becomes an impediment for participation in the society.
MAHER has identified a number of Generally Less Prioritised Diseases (GLPD) to focus on, based on the disease burden, availability of expertise, facilities and opportunities of treatment, as well as affordability. Orofacial clefting (OFC) is one such disease that describes a range of abnormalities that manifest in the newborn infant involving structures around the oral cavity and facial structures resulting in oral, facial and craniofacial deformity.
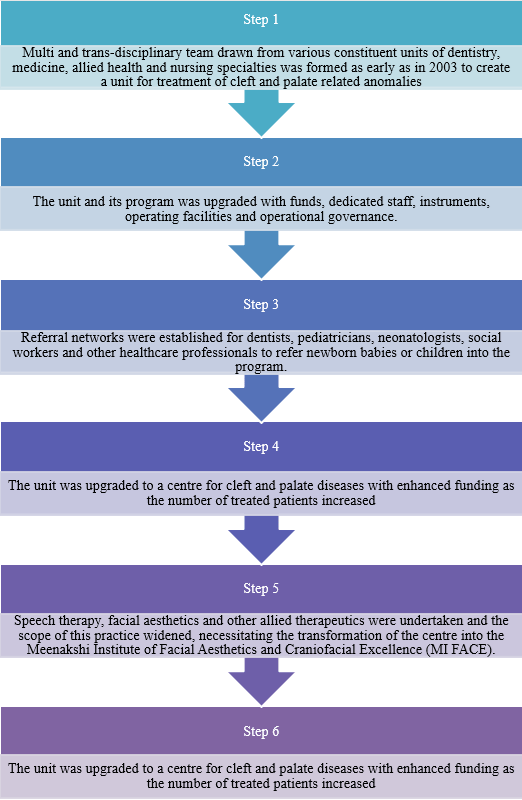
The primary challenge in the treatment of OFC is that it requires collaboration and cooperation from a wide range of specialisation, beginning with pre-marriage genetic counselling, prenatal screening, obstetric care, neonatal management, pediatric surgery, investigations, etc etc. In India, absence of births defects registry leads to paucity of data. The secondary challenge in OFC is the lack of standardised protocol for standard of care and surgical treatment, since there is an acute lack of sound evidence base. OFC requires follow up care throughout childhood into adulthood. Maintaining continuity of care and tracking of families has always been a challenge.
At MI FACE, these challenges have been tackled through establishment of multidisciplinary teams, project management principles and innovative patient data management systems in addition to evolving unique standard operating procedures and protocols, that are well documented, studied and improved upon. MI FACE today is a centre of excellence that serves as a sustainable model being replicated for other similar diseases in India and South Asia.
Our Success:
At MI FACE, over 8000 patients have benefited from the sustained focus and attention on OFC.
The Centre drew international attention due to its high profile successes, and was approached by the ‘Cleft Children International, Zurich, Switzerland’ for collaboration in the year 2003. Till date, more than 10,000 patients have benefited.
Research into OFC at the institute has resulted in publication of over 1000 articles, scientific papers in various high impact factor journals. A textbook on OFC is ready for publication. The Institute is now recognised widely for its expertise in treatment of OFC and attracts patients from all over India, even from far eastern states of Assam and Tripura, which attests to the impact of the institute’s work on the disease.